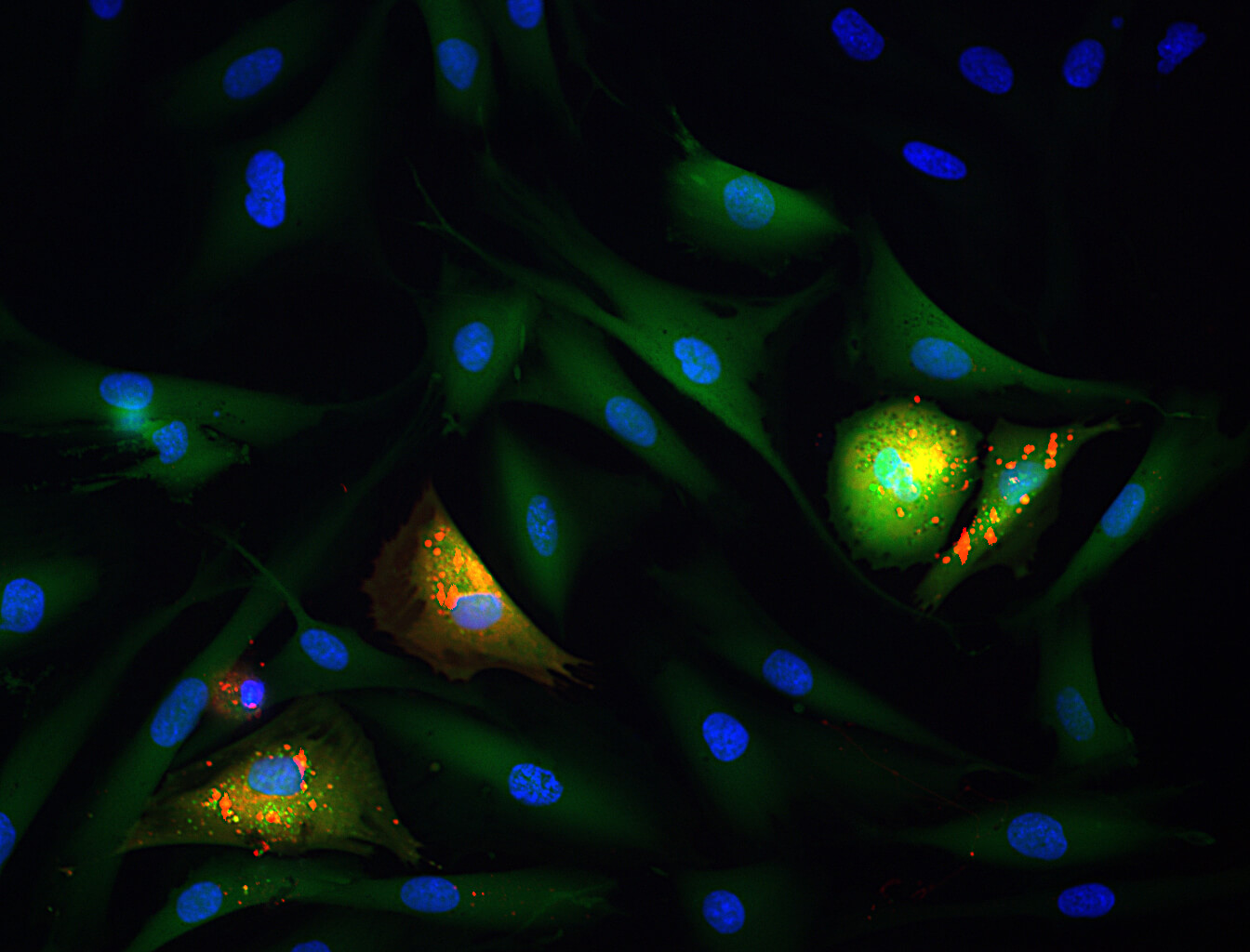
Aegle is developing novel therapies using bone marrow mesenchymal stem cell (MSC)-derived extracellular vesicles (EVs) to treat disorders with significant unmet medical need.
Our proprietary EV harvesting technology has the potential to develop therapies in multiple therapeutic areas. We are initially developing AGLE-102TM as a first-in-class therapy for a rare, monogenetic, pediatric disease called dystrophic epidermolysis bullosa (DEB). Aegle’s Phase 1/2 clinical trial involving AGLE-102 in individuals living with Recessive Dystrophic Epidermolysis Bullosa (RDEB) is now open for enrollment.
Pipeline
Discovery
Preclinical
Ind
Phase 1/2A
Dystrophic Epidermolysis Bullosa (AGLE-102)
Burns
Graft vs. Host Disease
Dystrophic Epidermolysis Bullosa
Epidermolysis bullosa (EB) is a group of rare, pediatric genetic disorders that manifests as blistering or erosion of the skin in response to little or no apparent trauma. While there are many genetic and symptomatic variations of EB, the disease is always painful, often pervasive and debilitating, and can dramatically reduce lifespan. Standard treatment for EB patients is daily bandaging and pain management. There is no treatment or cure for EB.
Dystrophic epidermolysis bullosa (DEB) is one of the major forms of EB. While there are several subtypes of DEB, they share the majority of symptoms and they are all caused by mutations in the same gene, COL7A1.
COL7A1 is a gene that is responsible for producing type VII collagen, which plays an important role in strengthening and stabilizing the skin. COL7A1 mutations alter the structure or disrupt the production of type VII collagen, which prevents the establishment of the necessary connection of the epidermis (top layer of skin) to the dermis (underlying layer). When type VII collagen is abnormal or missing, minor friction or trauma can cause the skin to separate, which leads to the formation of blisters and extensive scarring.
AGLE-102 contains COL7 protein as well as COL7A1 mRNA, which in preclinical models stimulates recessive DEB cells (cannot make any COL7) to produce COL7. AGLE-102 has the potential to induce functional regeneration and organization of complex tissue structures in DEB and EB patients that can potentially accelerate and enhance healing, reduce scarring, and improve overall cosmesis (McBride et al. 2018). In addition, AGLE-102 is non-immunogenic and carries the immunomodulating and anti-inflammatory properties of MSCs. Aegle’s Phase 1/2 clinical trial involving AGLE-102 in individuals living with Recessive Dystrophic Epidermolysis Bullosa (RDEB) is now open for enrollment. For more information regarding the trial, please read our Informational Brochure or visit ClinicalTrials.gov.
Burns/Scarring
In addition to DEB, Aegle’s IND for severe second-degree burns has been cleared by the FDA. A Phase 1 trial (NCT05078385) titled “A Pilot Safety Study of Mesenchymal Stem Cell Derived Extracellular Vesicles for the Treatment of Burn Wounds” is currently enrolling participants. This trial is planned to enroll a total of 10 patients and will evaluate accelerated healing, scarring, hair growth, re-pigmentation, and wound progression in severe second degree burn patients. This trial is funded by a grant from the Department of Defense. More information regarding this trial can be found on ClinicalTrials.gov.
Additional Indications
Aegle’s platform EV harvesting technology has the potential to treat a wide range of other therapeutic indications. Preclinical animal models have produced compelling data supporting the use of AGLE-102 for Graft vs. Host Disease prophylaxis. We are also evaluating other severe dermatological rare diseases associated with genetic protein deficiencies, as well as treatments for surgical wounds and graft sites. We believe AGLE-102 has the potential to be a safe and efficacious therapy in many indications where MSCs have shown therapeutic benefit.
Expanded Access Policy
Aegle Therapeutics Corporation (Aegle) is developing a first-in-class therapy using extracellular vesicles secreted by allogeneic bone marrow derived mesenchymal stem cells to treat rare diseases, including dystrophic epidermolysis bullosa, a rare pediatric blistering disease. Our clinical development resources are focused on conducting clinical studies required by the U.S. Food and Drug Administration (FDA) and regulatory authorities to obtain data on safety and efficacy that may be used to support approval of the product and subsequent wider accessibility to patients.
We share the urgency of patients seeking new treatments for potentially life-altering diseases and understand the interest in accessing our therapies outside of clinical trials and prior to regulatory approval. Expanded access, also referred to as compassionate use, is a channel through which the FDA allows physicians to request investigational medicines for patients. We do not currently offer any expanded access programs given that we are focusing our resources on development, clinical trials, and regulatory approval. We encourage patients who are interested in accessing therapies in our pipeline to talk to their doctor about participating in a clinical trial. Information about all our trials, including eligibility and locations, is available at ClinicalTrials.gov.
If we are able to offer expanded access in the future, we will update this policy. If you have further questions, please email us at info@AegleTherapeutics.com.